Benign Prostatic Hyperplasia (BPH) is the most common prostate condition affecting men, particularly as they age.
In the United States, over 50% of men over 50 experience symptoms of BPH, and this number rises to 90% by age 85.
BPH is closely linked with male lower urinary tract symptoms (LUTS), but it does not raise the risk of prostate cancer or cause sexual dysfunction. However, it can affect quality of life by leading to bothersome and sometimes embarrassing urinary issues.
While age and genetics play a key role in the development of BPH, emerging research shows that modifiable factors, including hormone levels, obesity, glucose regulation, diet, exercise, and inflammation, also influence its onset and progression.
Therefore, understanding these risk factors, recognizing early symptoms, and seeking timely diagnosis and treatment can dramatically improve outcomes and quality of life.
This article provides an overview of BPH, including its causes, symptoms, risk factors, diagnosis, and the latest treatment options, to help patients and caregivers understand how to manage this common condition effectively.
What is Benign Prostatic Hyperplasia?
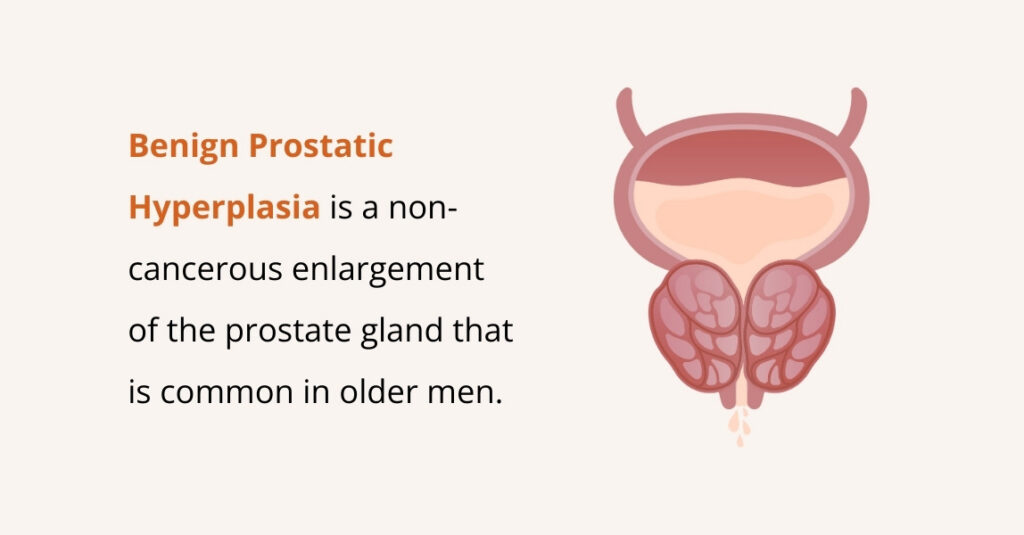
BPH is the non-cancerous enlargement of the prostate gland, a small walnut-sized organ below the bladder that surrounds the urethra and produces seminal fluid.
As men age, the prostate can enlarge from the size of a walnut to that of a lemon. In BPH, the prostate undergoes increased cell growth (hyperplasia), especially around the urethra, leading to gland enlargement.
As it grows, it can compress the urethra and partially block urine flow, causing symptoms such as difficulty starting urination, a weak urine stream, or needing to urinate frequently.
Who is more likely to have Benign Prostatic Hyperplasia?
In the United States alone, BPH accounts for millions of healthcare visits each year, reflecting its prevalence among an aging male population.
Certain risk factors make someone more prone to developing BPH:
- Age
Advancing age is the strongest risk factor. BPH is uncommon before 40, but the incidence rises sharply in later decades. The prostate tends to keep growing as men get older, which is why BPH primarily affects middle-aged and older men.
- Family History (Genetics)
Men with a family history of BPH, such as a father or brother who had an enlarged prostate, are more likely to develop the condition themselves. Studies have shown that first-degree relatives of BPH patients may have a fourfold increase in risk compared to men with no family history.
- Diabetes and Heart Disease
Research shows that chronic health conditions like type 2 diabetes and cardiovascular disease have been linked to a higher likelihood of BPH. Men with diabetes, in particular, have a higher incidence of BPH and often more severe symptoms, possibly due to insulin and growth-factor effects on the prostate.
- Diet and Obesity
An unhealthy diet and obesity can increase BPH risk. Research suggests that diets high in fat and red meat are associated with a greater risk of symptomatic BPH, whereas diets rich in vegetables may be protective. Obesity is also correlated with BPH; men who are overweight or who have metabolic syndrome tend to have larger prostate volumes and more symptoms.
- Localized Inflammation
Chronic prostatitis or inflammation of the prostate is often found alongside BPH on tissue analysis, and researchers suspect that inflammation may contribute to prostate enlargement. Inflammatory cells in the prostate can release factors that stimulate growth.
- Metabolic Syndrome
Related to the above factors, metabolic syndrome (a cluster of conditions including insulin resistance/diabetes, high blood pressure, and high cholesterol) has been linked to BPH.
Men with metabolic syndrome tend to have larger prostates on average, and those with poor blood sugar control have an increased risk of LUTS.
This may be due to metabolic syndrome’s association with obesity, inflammation, and hormonal imbalances that also drive prostate growth.
- Hormone Levels
Although not a traditional risk factor in the sense of a lifestyle choice, age-related hormonal changes underlie BPH development.
Research shows that men who have normal testes producing testosterone can develop BPH, whereas men who were castrated or have very low testosterone from a young age do not develop BPH.
What Causes Benign Prostatic Hyperplasia?
Despite how common BPH is, its exact cause remains unclear. As men grow older, changes in sex hormones, particularly the accumulation of dihydrotestosterone (DHT), can stimulate prostate growth.
Key factors contributing to BPH:
- Aging
- Hormonal changes
- Family history
- Lifestyle factors
Other health conditions, such as obesity, type 2 diabetes, and heart and blood vessel diseases
What are the Symptoms of Benign Prostatic Hyperplasia?
BPH mainly affects urination and can range from mild to severe. As the prostate enlarges, it presses on the urethra and bladder, leading to lower urinary tract symptoms (LUTS) that can disrupt daily life.
Common BPH symptoms include:
- Frequent urination: Needing to urinate more often, especially at night (nocturia). Some men go every 1–2 hours.
- Urgency: A sudden, strong urge to urinate, even when the bladder isn’t full.
- Difficulty starting urination (hesitancy): Trouble beginning the urine stream, sometimes requiring straining.
- Weak or interrupted urine stream: A slow or stop-and-start flow due to urethral narrowing.
- Dribbling at the end: Small drops of urine may continue after finishing.
- Incomplete bladder emptying: Feeling that the bladder isn’t fully emptied, leading to frequent trips to the bathroom.
- Urinary retention: In severe cases, partial or complete blockage can make urination difficult or impossible, which is a medical emergency.
- Painful urination (dysuria): BPH itself usually doesn’t cause burning, but infections or straining can.
- Blood in the urine (hematuria): Straining or bladder irritation can cause small amounts of blood in the urine; a doctor should check any visible blood.
Many of these symptoms are quantified by doctors using the International Prostate Symptom Score (IPSS), which is a questionnaire that asks about frequency, nocturia, weak stream, etc., to grade symptom severity from mild to severe.
Also, not every man with BPH will have all these symptoms, and the severity can vary.
What are the Complications of Benign Prostatic Hyperplasia?
BPH is benign and usually develops slowly, but if it becomes advanced or is left untreated, it can lead to complications in the urinary tract.
The prostate’s blockage of urine flow and the resulting strain on the bladder can cause several issues:
- Urinary Retention: The enlarged prostate can block urine flow, causing the bladder to fill and sometimes leading to sudden, painful inability to urinate (acute retention) or constant partial retention.
- Recurrent Urinary Tract Infections (UTIs): When the bladder doesn’t empty fully, urine can stagnate, leading to infections and symptoms such as burning, cloudy urine, or pelvic pain.
- Bladder Stones: Minerals in leftover urine can form stones, which may worsen urinary problems or cause blood in the urine.
- Bladder Damage: Constant pressure on the bladder can weaken its muscles and reduce its ability to empty properly. This can cause long-term urinary problems even after treatment.
- Kidney Damage: Severe blockage can cause urine to back up into the kidneys (hydronephrosis), potentially leading to kidney injury or infection. Rarely, untreated BPH can contribute to kidney failure.
- Incontinence: Overflow or urge incontinence can occur when the bladder is too full or unstable. Some BPH treatments may also cause temporary incontinence.
- Blood in Urine (Hematuria): Persistent bleeding can happen due to the enlarged prostate, sometimes requiring treatment.
- Sexual Side Effects: BPH itself doesn’t cause erectile dysfunction, but treatments may lead to issues like retrograde ejaculation, which can affect fertility but is not dangerous.
Many of these complications are preventable with timely treatment. If you have BPH, it’s important to follow up with your healthcare provider, especially if symptoms are worsening.
How is Benign Prostatic Hyperplasia Diagnosed?
When BPH is suspected, healthcare providers will perform a series of evaluations to confirm the diagnosis, assess severity, and rule out other conditions (like infections or prostate cancer) that can cause similar symptoms.
Diagnosing BPH typically involves some or all of the following steps and tests:
- Medical history & symptom check: Your doctor will ask about urinary habits (frequency, urgency, nighttime trips, stream changes, blood in urine) and may use a questionnaire such as the IPSS/AUA symptom score to rate severity.
- Digital rectal exam (DRE): A quick exam where the doctor feels the prostate through the rectal wall to estimate size and check for lumps or hard areas.
- Urinalysis: A urine sample checks for infection, blood, or other conditions (e.g., diabetes) that can mimic or worsen symptoms.
- PSA blood test: Measures prostate-specific antigen. PSA can be higher with larger prostates or cancer, so results are interpreted alongside other findings.
- Uroflowmetry (flow test): You urinate into a device that measures flow rate and volume to see if there’s an obstruction.
- Post-void residual (PVR) scan: A quick bladder ultrasound (or catheter measurement) shows how much urine remains after voiding—high volumes suggest incomplete emptying.
- Transrectal ultrasound (TRUS): Used when precise prostate size is needed (for treatment planning) or before biopsy; not required in every case.
- Cystoscopy: A scope is passed into the urethra to view the prostate and bladder directly; it is used when symptoms are unusual or before certain procedures.
- Urodynamic testing: Specialized pressure and flow studies that evaluate bladder function; reserved for complex cases (e.g., weak bladder muscle, neurologic disease).
- Advanced imaging (MRI/CT): Not routine for BPH, but may be used if cancer is suspected or to assess the kidneys/bladder when complications are possible.
In most cases, a combination of history, DRE, urinalysis, PSA, and simple office tests (uroflow and PVR) is enough to diagnose BPH and start treatment.
More invasive or specialized tests are used when the diagnosis is uncertain, symptoms are severe, or surgery is being considered.
Benign Prostatic Hyperplasia Treatment Options
Multiple treatment options exist for BPH, ranging from simple lifestyle adjustments to medications to minimally invasive procedures and surgery.
Here we’ve outlined the main categories of BPH treatment:
Lifestyle Changes (Conservative Management)
For men with mild BPH symptoms, simple lifestyle adjustments can help reduce urinary problems and improve comfort:
- Adjust fluid intake: Avoid drinking large amounts in the evening and limit fluids 1–2 hours before bedtime to reduce nighttime bathroom trips.
- Limit bladder irritants: Cut back on caffeine, alcohol, and any foods that trigger bladder irritation, such as spicy or acidic items.
- Stay active and maintain a healthy weight: Regular exercise (e.g., 30 minutes of brisk walking daily) can improve urinary symptoms. Maintaining a healthy weight, blood pressure, and blood sugar also supports prostate health.
- Optimize bathroom habits: Urinate when you feel the urge, and try “double voiding” to empty the bladder more completely. Planning regular trips every 2–3 hours can help manage frequent urges.
- Review medications: Some decongestants, antihistamines, and diuretics can worsen urinary symptoms. Consult your doctor before using these medications.
- Pelvic floor exercises: Kegel exercises can strengthen the pelvic muscles and improve bladder control.
- Stay warm: Cold can worsen urinary retention; dressing warmly and avoiding prolonged exposure to cold may help.
Many men start with “watchful waiting” using these habits, often managing symptoms without medication. Regular check-ups are important to monitor progression.
If symptoms worsen, doctors may recommend medications or other treatments.
Medications for BPH
For men with moderate to severe BPH, medications are usually the first line of treatment. These drugs either relax the prostate and bladder muscles to improve urine flow or shrink the prostate over time.
Common options include:
- Alpha-blockers
These relax the muscles in the prostate and bladder neck, making urination easier. They work quickly (days to weeks) but do not shrink the prostate.
- 5-Alpha-Reductase Inhibitors (5-ARIs)
Drugs like finasteride (Proscar) and dutasteride (Avodart) shrink the prostate by blocking DHT, the hormone that drives growth. They take several months to work and are most effective in larger prostates.
- Combination Therapy
For men with severe symptoms or large prostates, alpha-blockers and 5-ARIs can be used together (e.g., tamsulosin + dutasteride, Jalyn®). This provides fast symptom relief and long-term prostate shrinkage.
- Phosphodiesterase-5 inhibitors (PDE-5i)
Tadalafil (Cialis) at a low daily dose can improve urinary symptoms by relaxing the bladder and prostate muscles. It’s especially helpful for men who also have erectile dysfunction.
- Other Medications
For overactive bladder symptoms, anticholinergics (e.g., oxybutynin, tolterodine) or beta-3 agonists (mirabegron) may be added. These help reduce urgency and frequency but must be used carefully if bladder emptying is poor.
Most men start with an alpha-blocker for quick relief. If the prostate is large or symptoms persist, a 5-ARI or combination therapy may be added.
Doctors monitor symptom scores, urine flow, and PSA levels to ensure treatment is effective and safe. If medications don’t work or side effects are unacceptable, minimally invasive procedures or surgery may be considered.
Minimally Invasive Procedures for BPH
For men whose symptoms aren’t fully controlled with medication or who want to avoid major surgery, minimally invasive procedures offer effective alternatives with quicker recovery and fewer complications.
These procedures either widen the urethra or shrink prostate tissue. Common options include:
- Prostatic Artery Embolization (PAE)
Prostatic artery embolization is a truly minimally invasive, non-surgical procedure performed by Dr. Zagum Bhatti, an interventional radiologist.
It involves accessing the blood vessels to the prostate (usually via a catheter inserted in the femoral or radial artery) and injecting tiny particles to block blood flow in the prostatic arteries.
PAE is done under local anesthesia and sedation, and typically, no hospital stay is needed.
It’s an option for men who may not tolerate surgery or anesthesia or who prefer an arterial approach. PAE’s advantages are that there’s no incision, no general anesthesia, and sexual function is generally preserved.
- Prostatic Urethral Lift
This is a device-based therapy where small implants are used to pull apart the enlarged prostate lobes, widening the urethral passage.
The urologist inserts a special instrument through the urethra and places several tiny spring-like implants that tether the prostate lobes open, almost like curtain tie-backs, to prevent them from pressing inward. This does not involve cutting or destroying tissue, and it can be done under local anesthesia or light sedation.
The benefit is that it improves urine flow and often preserves sexual function (minimal risk of retrograde ejaculation or ED) compared to traditional surgery. It is best suited for men with relatively moderate prostates and no large middle lobe.
- Rezūm Water Vapor Therapy
Rezūm is a newer treatment that uses steam injections to ablate prostate tissue.
During this procedure, a device is introduced via the urethra and a small needle is deployed into the prostate; steam (water vapor) is then released, which delivers thermal energy that kills the surrounding prostate cells.
Over the next days and weeks, the body’s immune system clears away the treated tissue, shrinking the prostate.
- Laser Therapy
Laser prostatectomy involves inserting a scope through the urethra and using laser energy to burn/vaporize or cut prostate tissue.
Examples include photoselective vaporization of the prostate (PVP), often called GreenLight laser (which vaporizes tissue), and holmium laser enucleation of the prostate (HoLEP), which uses a laser to actually enucleate (carve out) the enlarged prostate tissue in lobes.
The advantage of lasers: lower risk of bleeding, so it’s good for patients on blood thinners or with bleeding risks. However, side effects like retrograde ejaculation still occur in many cases (especially if a lot of tissue is removed).
- Transurethral Microwave Therapy (TUMT)
This is an older minimally invasive therapy where a special catheter with a microwave antenna is inserted into the urethra, and microwave energy heats and destroys prostate tissue from inside.
TUMT can be done without general anesthesia. It generally only reduces symptoms moderately and may take weeks to have an effect.
Surgical Procedures
Modern BPH surgeries are mostly done endoscopically (through the urethra) without external cuts, providing lasting relief by removing or reducing the enlarged prostate tissue.
Common surgical options include:
- Simple Prostatectomy (Open or Robot-Assisted)
Reserved for very large prostates (>80–100 grams), this involves removing the enlarged internal portion via an open incision or robot-assisted surgery.
Recovery is longer, with a few days in the hospital and the use of a catheter. It carries higher risks like bleeding, infection, and blood clots, but offers excellent symptom relief.
- Transurethral Incision of the Prostate (TUIP)
TUIP is for men with small prostates (<30 cc) but significant blockage. The surgeon makes one or two small cuts in the prostate and bladder neck to widen the urethra without removing tissue.
Recovery is usually quick, with a lower risk of retrograde ejaculation than TURP.
In general, surgery is considered when symptoms are severe and not responding well to meds, the patient can’t tolerate meds, or if there are complications.
How to Prevent Benign Prostatic Hyperplasia
Since BPH is so tied to the aging process and genetics, there is no guaranteed way to prevent prostate enlargement altogether.
Here are some strategies that may help support long-term prostate health:
- Eat a Healthy Diet: Focus on fruits, vegetables, whole grains, and healthy fats (such as fish, nuts, and olive oil). Avoid too much red meat, high-fat foods, processed foods, sugar, and excess dairy.
- Maintain a Healthy Weight: Obesity can disrupt hormone balance and increase the risk of BPH. Staying at a healthy weight through diet and exercise may help prevent prostate enlargement.
- Exercise Regularly: Aim for at least 30 minutes of moderate activity, like walking, most days. Exercise improves blood flow and hormone balance and reduces inflammation, all of which support prostate health.
- Manage Chronic Health Conditions: Keep diabetes, high blood pressure, and cholesterol under control. Good metabolic health may lower the risk of BPH progression. Avoid smoking, as it can worsen urinary symptoms.
- Avoid Irritants: Limit caffeine and alcohol, especially in the evening, to reduce bladder stress. Stay hydrated but avoid extremes of too little or too much fluid.
- Preventive Medications (for select cases): In certain men at higher risk (strong family history or early prostate enlargement), doctors may sometimes consider low-dose 5-alpha-reductase inhibitors to slow growth. This is not routine for all men.
Remember, BPH is common with age, but a healthy lifestyle can delay symptoms, reduce severity, and improve well-being.
Frequently Asked Questions (FAQs)
How common is Benign Prostatic Hyperplasia?
BPH is very common, especially as men get older.
While many men may have an enlarged prostate (even without symptoms), a large portion of older men will experience BPH to some degree.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), BPH affects 5–6% of men aged 40–64, and 29–33% of men aged 65 and older. Similarly, Johns Hopkins Medicine estimates that about 1 in 4 men by age 55 have symptoms, and about 50% of men by age 75 do.
Can an enlarged prostate be cured?
An enlarged prostate can be treated with medications like 5-ARIs and procedures such as Prostatic Artery Embolization, relieving blockage and symptoms, often for many years. Since BPH is linked to aging, the prostate may grow again over time, but symptoms are usually well controlled. With proper treatment, follow-up, and healthy habits, most men regain normal urinary function and quality of life.
What happens if you leave an enlarged prostate untreated?
If an enlarged prostate (BPH) is left untreated, symptoms can gradually worsen and lead to serious problems: urine may not empty fully or you can suddenly be unable to urinate (acute urinary retention), recurrent urinary tract infections and bladder stones can develop, and long-term bladder strain can weaken the bladder. In severe cases, urine can back up into the kidneys (hydronephrosis) and cause kidney damage, and visible blood in the urine or new incontinence may occur. These issues reduce quality of life and can become medical emergencies.
How long can I live with an enlarged prostate?
You can live a long, healthy life with an enlarged prostate (BPH), as it is noncancerous and doesn’t raise the risk of prostate cancer. Life expectancy isn’t affected when symptoms are managed with lifestyle changes, medications, or procedures such as Prostatic Artery Embolization. Untreated BPH can worsen over time, but many men with mild symptoms live comfortably for years while managing them.
What type of doctor treats benign prostatic hyperplasia?
A urologist is the primary specialist for BPH, managing both medications and procedures such as Prostatic Artery Embolization. Primary care doctors can evaluate early symptoms and start basic treatment, but significant or persistent BPH usually requires a urologist’s care.
Can BPH lead to prostate cancer?
No, BPH does not cause prostate cancer. It is a benign condition, and the prostate cells are not cancerous. BPH does not raise your risk of developing prostate cancer. However, because both conditions can cause similar symptoms, such as frequent or difficult urination, regular checkups are important to rule out cancer.
Conclusion
Benign Prostatic Hyperplasia is a very common and manageable condition that affects a great number of aging men.
While the prospect of an “enlarged prostate” can be worrisome, it’s important to remember that BPH is benign, it is not prostate cancer, and in itself is not life-threatening.
The primary impact of BPH is on quality of life: it can cause frustrating urinary symptoms that interrupt sleep, work, and daily comfort.
With modern medications and minimally invasive treatments, most men can find relief that suits their needs and lifestyle.
If you’re a man over 50 experiencing urinary changes, such as increased frequency, hesitancy, or nocturia, it’s important to talk to your healthcare provider.
That said, a simple evaluation can identify BPH as the cause and guide you to the most appropriate treatment plan.
Today, men don’t have to live with severe urinary problems like previous generations. Early consultation and personalized care can keep BPH a minor concern rather than a major obstacle to healthy aging.

Leave a Reply