For many expecting parents, the discovery of fibroids during a routine prenatal ultrasound comes as a surprise.
Fibroids are incredibly common, and in many cases, people don’t even know they have them until pregnancy brings them to light.
As more individuals choose to start families later in life, when fibroids naturally become more frequent, these findings are becoming part of the modern pregnancy experience.
While most pregnancies involving fibroids progress smoothly, their presence can raise understandable questions.
- Will they affect the baby’s growth?
- Increase the risk of preterm birth?
- Lead to pain or complications later in pregnancy?
The answers depend on factors like size, number, and location, and with the right monitoring, many people navigate pregnancy with fibroids without major issues.
In this guide, we’ll explain the impact of fibroids on pregnancy, outline potential risks, describe diagnostic approaches, and provide practical strategies for managing fibroids while pregnant.
How Fibroids Affect Pregnancy
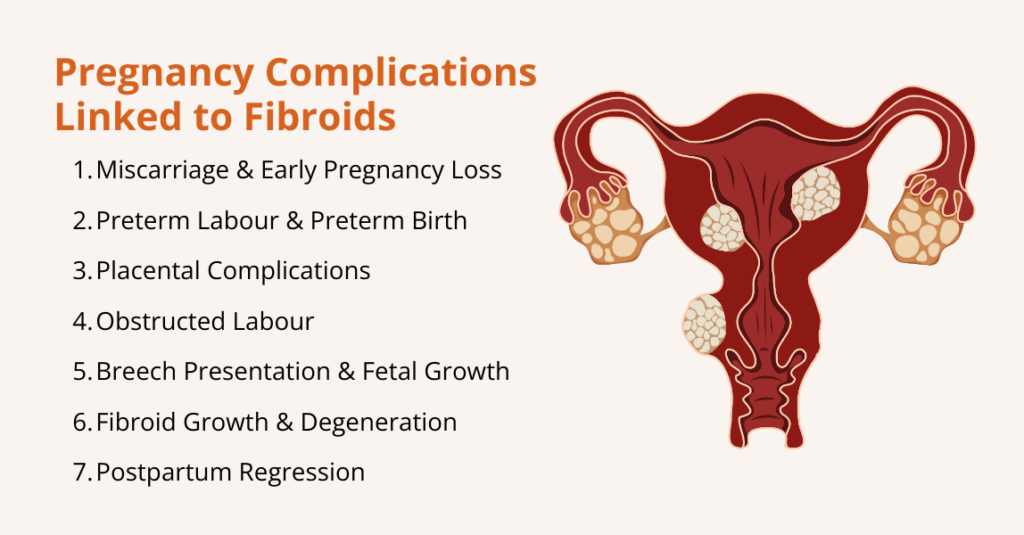
The presence of uterine fibroids (even when they’ve been harmless before pregnancy) can influence pregnancy in several ways, from early pregnancy loss to complications late in pregnancy or at delivery. The risks vary based on fibroid size, number, and location.
Here are some of the ways fibroids can influence pregnancy:
1. Miscarriage and Early Pregnancy Loss
Fibroids, particularly submucosal lesions, are associated with an increased risk of miscarriage.
A meta‑analysis pooling data from more than 237,000 participants found that women with fibroids had a higher risk of miscarriage than those without fibroids (relative risk RR ≈ 4.5, with miscarriage rates 13.42 % vs. 2.84 % in controls).
The risk is highest when fibroids distort the uterine cavity, because the altered blood supply and mechanical interference impair implantation and early placental development.
2. Preterm Labour and Preterm Birth
Large or multiple fibroids can irritate the uterus and trigger contractions, leading to preterm labour.
A study reported that preterm birth occurred in 12.85 % of pregnant patients with fibroids versus 9.43 % of controls; after adjusting for confounders, fibroids remained associated with preterm birth.
Another study estimated that 10 %–30 % of pregnant women with fibroids develop obstetric complications such as preterm labour. Also, premature uterine contractions may be due to local inflammation, degenerating fibroids, or increased uterine irritability.
3. Placental Issues
Fibroids can interfere with placentation. If a fibroid is located near the placenta, it may lead to:
- Placenta Previa: The placenta covers the cervix, obstructing the birth canal.
- Placental Abruption: Premature separation of the placenta. The meta‑analysis found an elevated risk of placental abruption in women with fibroids.
- Placenta Accreta Spectrum: Fibroids may increase the likelihood of abnormal placental attachment; however, the data remain limited.
4. Need for Caesarean Delivery
Large intramural or subserosal fibroids can physically obstruct the birth canal, preventing the fetal head from descending. Thus, fibroids raise the odds of cesarean delivery.
For example, fibroids growing low in the uterus or near the cervix may block the birth canal, preventing the baby’s head from descending.
Others may distort the uterus, making it harder for the baby to settle into a head-down position and leading to breech or transverse presentations.
5. Breech Presentation and Fetal Growth Restriction
Fibroids, especially those in the lower uterine segment, can distort the uterine cavity and limit space for the fetus. Research highlights that breech presentation or other fetal malposition is more common when fibroids are present, likely because fibroids can alter the shape of the uterine cavity.
Similarly, in analyses comparing by fibroid size, larger fibroids conferred especially high risk of breech presentation and placenta previa.
However, the overall effect on fetal growth remains uncertain because many pregnancies with fibroids result in normal birth weights.
6. Fibroid Growth and Degeneration during Pregnancy
Fibroids behave unpredictably during pregnancy.
A study describes a woman in early pregnancy who arrived with severe abdominal pain, which imaging later confirmed was caused by a degenerating fibroid. This degeneration occurs when a fibroid outgrows its blood supply, leading to tissue ischemia and necrosis.
7. Postpartum Regression
After delivery, many fibroids shrink as hormonal levels decline and the uterus involutes.
A case series found that fibroids decreased in size in 7% of women postpartum and that their volume could shrink by 5% within 6 months.
Ongoing breastfeeding may further promote fibroid regression. Another observational study reported that 37 % of fibroids disappeared postpartum and that breastfeeding was associated with fibroid regression.
What are the Risks and Complications of Fibroids during Pregnancy

While many women with fibroids have healthy pregnancies, these benign growths can sometimes create challenges as the uterus expands and hormonal changes intensify.
Here are the key complications associated with fibroids during pregnancy:
1. Premature Rupture of Membranes
Fibroids can cause uterine irritability, increasing the frequency of contractions and elevating the risk of preterm labour.
The high‑risk pregnancy resource notes that adverse outcomes such as preterm labour and premature rupture of membranes (PROM) are more common when fibroids exceed 10 cm.
The meta‑analysis reported that fibroids were associated with both preterm birth and preterm PROM. Continuous antenatal care with ultrasound monitoring can help detect early cervical changes and manage preterm labour, sometimes using medications such as tocolytics to delay delivery.
2. Heavy Bleeding Due to Placental Problem
Placental problems can cause heavy bleeding and require early delivery or caesarean section. Women with placenta previa are more likely to deliver via caesarean section.
Research shows that placenta previa may manifest as painless vaginal bleeding, often requiring bed rest or early delivery; placental abruption presents with painful bleeding and is an obstetric emergency.
Importantly, fibroids located near the placenta or in the lower uterine segment increase these risks.
3. Obstructed Labour
Large fibroids can obstruct the cervix or lower uterine segment. When the fibroid blocks the birth canal, a caesarean delivery becomes necessary.
Additionally, fibroids may cause dystocia (slow cervical dilation), prolonging labour and increasing the likelihood of operative delivery.
The High‑Risk Pregnancy Information site states that a caesarean section is six times more likely in women with fibroids, highlighting the need for careful intrapartum planning.
4. Postpartum Haemorrhage (PPH)
PPH is excessive bleeding after delivery, often due to uterine atony (failure of the uterus to contract). Fibroids can impede uterine contraction, particularly if they distort the uterine muscle or occupy the uterine wall.
The meta‑analysis found that postpartum haemorrhage occurred in 10.10 % of women with fibroids compared with 3.96 % in controls. Obstetric teams anticipate this risk and prepare for active management of the third stage of labour in women with known fibroids.
5. Preeclampsia and Other Hypertensive Disorders
Emerging evidence indicates a modestly increased risk of preeclampsia (new‑onset hypertension with end‑organ damage) in women with fibroids. The meta‑analysis reported an association between fibroids and preeclampsia.
Although the absolute increase is small, pregnant women with fibroids should be monitored for blood pressure changes.
6. Fetal Malpresentation and Growth Issues
Fibroids can affect how a baby positions itself in the uterus, sometimes leading to malpresentation, when the baby is not head-down at the time of delivery.
For example, large fibroids or those located near the lower uterine segment can physically block the baby from turning into the optimal head-first position, increasing the likelihood of breech or transverse presentation.
In addition, fibroids may influence fetal growth. Large or multiple fibroids can reduce the space available for the baby to grow or interfere with blood flow to the placenta, which can occasionally lead to fetal growth restriction (FGR).
While not all fibroids cause these issues, monitoring fetal position and growth via ultrasounds is crucial to ensure timely interventions if complications arise.
How to Diagnose Fibroids during Pregnancy?
Diagnosing fibroids during pregnancy can be challenging because the growing uterus often makes physical examination unreliable.
As a result, healthcare providers rely primarily on imaging to identify fibroids, determine their size, location, and number, and monitor any changes throughout pregnancy.
Here are the main diagnostic approaches:
- Ultrasound (US): Ultrasound is the primary tool for detecting fibroids during pregnancy. Using a transabdominal or transvaginal probe, providers can visualize the uterus, count fibroids, measure their size, and monitor growth. Ultrasound is safe because it uses sound waves rather than radiation.
- Magnetic Resonance Imaging (MRI): MRI provides detailed images of uterine tissue when ultrasound is unclear, for example, with large fibroids or fibroids behind the placenta.
- Other Tests: Techniques like X-ray, CT scans, hysterosalpingography, and sonohysterograms exist but are rarely used during pregnancy due to radiation exposure.
- Surgical Diagnosis: In rare cases when imaging cannot clearly differentiate fibroids from other uterine masses, laparoscopy or hysteroscopy may be performed to visualize the uterus directly. These procedures are generally avoided during pregnancy unless absolutely necessary.
Monitoring Fibroids during Pregnancy
Once diagnosed, fibroids are monitored regularly. Obstetricians often perform ultrasounds at 20 weeks, 32 weeks, and sometimes earlier if symptoms (pain, bleeding, rapid uterine growth) arise.
They assess fibroid size, location relative to the cervix and placenta, and signs of degeneration. Given this, frequent imaging helps detect complications such as placental abruption or fetal growth restriction in a timely manner.
How to Deal with Fibroids during Pregnancy?
Managing fibroids during pregnancy focuses on monitoring for complications, controlling pain, modifying activities, and maintaining overall health.
Here are some of the most common ways to deal with fibroids during pregnancy:
Monitoring and Regular Check-Ups
Once fibroids are diagnosed during pregnancy, ongoing monitoring is essential to ensure both maternal and fetal health.
Regular check-ups help track fibroid growth, assess fetal development, and identify potential complications early. Here’s how:
- Routine Ultrasounds: These are performed periodically to track fibroid size, monitor fetal growth, and detect issues such as placental problems or cervical shortening.
- MRI when indicated: If ultrasound images are unclear, particularly with large, multiple, or posteriorly located fibroids, MRI can provide more detailed information without radiation exposure.
- Fetal Growth Assessments: Serial ultrasounds measure fetal size to identify intrauterine growth restriction (IUGR). If growth concerns arise, obstetricians may adjust delivery planning to ensure optimal outcomes.
- Cervical Length Monitoring: Transvaginal ultrasounds measure cervical length, and if the cervix is short, treatments such as progesterone supplementation or cervical cerclage may be recommended.
Regular monitoring ensures that both the mother and baby are closely observed throughout pregnancy, allowing healthcare providers to respond quickly to any complications related to fibroids.
Pain Management
Managing pain safely is crucial to protect both the mother and the developing baby. Treatment strategies should balance effective relief with fetal safety.
If pain or discomfort occurs, acetaminophen (paracetamol) is one of the safest options. According to the American College of Obstetricians and Gynecologists (ACOG), when used as needed, at the lowest effective dose, and for the shortest possible time, acetaminophen remains the preferred pain and fever medicine in pregnancy.
Untreated pain or fever itself can pose risks to a developing baby, so controlling pain wisely matters.
Also, the U.S. Food and Drug Administration (FDA) warns that using NSAIDs after about 20 weeks can harm the baby’s kidneys, reduce the fluid around the baby (amniotic fluid), and lead to serious complications.
Because of these risks, NSAIDs like ibuprofen or naproxen should generally be avoided after mid‑pregnancy, unless a doctor says otherwise.
For mild pain, non‑medication options can also help. Simple measures, such as warm compresses, warm baths or showers, a pregnancy support belt, gentle stretching or prenatal yoga, and rest, can safely ease discomfort.
Activity Modifications
Making thoughtful adjustments to daily activities can help reduce discomfort from fibroids and support a healthy pregnancy.
Gentle modifications, along with proper rest and nutrition, play a key role in managing symptoms safely. Here are the practical tips for activity and lifestyle:
- Low-impact exercise: Avoid heavy lifting or high-impact workouts; choose walking, prenatal yoga, or swimming.
- Rest and stress management: Use mindfulness, meditation, or prenatal massage to reduce discomfort.
- Hydration and diet: Eat a high-fiber, nutrient-rich diet and stay hydrated to prevent constipation and pelvic pressure.
These simple changes help ease symptoms and promote maternal and fetal well-being.
Rest and Stress Reduction
Managing stress and getting adequate rest are important for easing fibroid-related discomfort during pregnancy.
- Relaxation Techniques: Practices such as prenatal yoga, deep breathing exercises, and mindfulness can help reduce stress and relieve pelvic or abdominal discomfort caused by fibroids.
- Adequate Rest: Prioritizing sufficient rest allows the body to recover, lowers physical strain, and helps minimize pain, especially when fibroids contribute to pelvic pressure.
Incorporating these habits can improve overall comfort and support a healthier pregnancy experience.
Diet and Hydration
Good nutrition and plenty of fluids can ease fibroid-related discomfort and support a healthy pregnancy.
- Balanced diet: Eat regular, nutrient-rich meals with plenty of fiber, fruits, vegetables, legumes, and whole grains, plus lean protein and healthy fats. Fiber helps prevent constipation, which can worsen pelvic pressure from fibroids.
- Staying hydrated: Drink water throughout the day to support digestion and circulation; staying well hydrated also helps reduce constipation and general discomfort.
Together, a fiber-rich diet and consistent hydration help manage everyday stress and support overall maternal and fetal health.
Frequently Asked Questions (FAQs)
Do fibroids affect pregnancy?
No. Most women with fibroids have normal pregnancies, particularly when fibroids are small or located away from the uterine cavity. The High‑Risk Pregnancy Information site estimates that only 10 %–30 % of pregnant women with fibroids develop complications. Nevertheless, because complications can be serious, women with fibroids should have enhanced prenatal care.
Can fibroids cause pain during pregnancy?
Yes, fibroids can cause pain during pregnancy, and it is the most common symptom associated with these growths. Pain often appears in the second or third trimester when fibroids grow faster than their blood supply, leading to a condition called red degeneration (also known as carneous degeneration). Fibroid pain may also result from mechanical pressure on nearby organs or from torsion of a pedunculated fibroid. Most mild pain can be safely managed with acetaminophen and rest. However, severe or persistent abdominal pain should prompt immediate medical evaluation, as it may indicate complications such as fibroid degeneration, placental issues, or preterm labour.
Do fibroids grow during pregnancy?
Yes, fibroid growth can occur during pregnancy, but patterns vary depending on the size and location of the fibroid. Many fibroids tend to grow in the first trimester due to rising estrogen and progesterone levels. Research shows that small fibroids (less than 1 cm) often increase in volume, medium-sized fibroids usually remain stable, and large fibroids (3 cm or more) may actually shrink. Interestingly, about 10–12% of fibroids regress spontaneously during pregnancy.
Do fibroids shrink after pregnancy?
Yes, many fibroids shrink postpartum. A case series found that fibroid size decreased in 72 % of women after giving birth and that fibroid volume could decrease by 50 % within six months. The postpartum uterus contracts to its pre‑pregnancy size, and hormonal changes (lower estrogen and progesterone levels) contribute to fibroid regression. Breastfeeding may enhance regression. However, some fibroids persist or regrow over time, so postnatal follow‑up is important.
Conclusion
Fibroids are common benign tumors that often coexist with pregnancy. For the majority of women, fibroids will not significantly impact fertility or pregnancy outcome.
Nevertheless, fibroids can increase the risk of miscarriage, preterm labour, placental complications, caesarean delivery, breech presentation, and postpartum haemorrhage.
Comprehensive prenatal care, including regular ultrasounds, growth monitoring, and blood pressure screening, allows obstetricians to detect complications early and implement appropriate interventions.
The safest pain management strategy during pregnancy is to use acetaminophen judiciously after consulting a healthcare professional; NSAIDs should generally be avoided after 20 weeks because they can reduce amniotic fluid and harm the fetus.
Non‑pharmacologic measures such as rest, gentle exercise, hydration, and stress reduction can help alleviate discomfort. Most fibroids regress after birth, especially with breastfeeding.
Given this, women with fibroids should work closely with their healthcare team to develop a personalized care plan.

Leave a Reply