Infertility is a common medical condition that can also be deeply stressful and emotionally painful for individuals and couples.
But you are not alone. It is more common than many people realize.
According to the CDC, 1 in 5 (19%) of married women aged 15 to 49 in the U.S. with no prior births are unable to get pregnant after 1 year of trying.
Studies suggest that after 1 year of having unprotected sex, 12% to 15% of couples are unable to conceive, and after 2 years, 10% of couples still have not had a live-born baby.
Infertility is not only a “woman’s problem.”
Causes may arise from the female side or from the male side. Many couples have mixed or unexplained factors, which is why evaluating both partners is standard practice.
Some causes of infertility are preventable. Medications or assisted reproductive technologies are aimed at maximizing the chances of conception.
In this guide, you’ll gain an understanding of what infertility is, its types, causes, signs and symptoms, diagnoses, and available treatment options.
What is Infertility?
According to the World Health Organization (WHO), infertility is a disease of the male or female reproductive system defined by the failure to achieve a pregnancy after 12 months or more of regular unprotected sexual intercourse.
Conception requires a series of coordinated steps: a mature egg released during the ovulation portion of the menstrual cycle, sperm reaching and fertilizing the egg (typically in the fallopian tube), formation of an embryo, and successful embryo implantation in a receptive uterine lining.
Disruption at any step, irregular or absent ovulation (menstrual cycle dysregulation), poor egg quality or reduced ovarian reserve, impaired sperm quality (count, shape, motility), tubal blockage, or uterine factors, can cause infertility.
What are the Types of Infertility?
Infertility affects millions of people and has an impact on their families and communities.
WHO estimates suggest that approximately one in every six people of reproductive age worldwide experiences infertility in their lifetime.
Types of infertility include:
1. Primary Infertility
This refers to a person or couple who have never achieved a pregnancy (or live birth) despite at least 12 months of regular, unprotected intercourse (or 6 months if the woman is 35 or older).
Because no prior conception has occurred, the evaluation typically begins once the diagnostic threshold (12 or 6 months) is reached.
Also, there is no prior successful pregnancy history; clinicians often consider a full infertility work-up (ovulation assessment, ovarian reserve, tubal/uterine imaging, semen analysis) more promptly.
The absence of prior conception may suggest more significant or multiple contributing factors.
2. Secondary Infertility
It occurs when a person or couple has had at least one prior pregnancy (regardless of outcome) but is now unable to conceive after the defined interval of regular unprotected intercourse.
Because a prior conception occurred, some systems (ovulatory, tubal, sperm) were once functional. The evaluation may focus on “what changed.”
For example, age-related decline in ovarian reserve, new tubal damage, and a change in partner sperm quality.
Therefore, prompt assessment is required, especially if age or other risk factors are present. Still, the perceived urgency is sometimes slightly less than in primary infertility (depending heavily on age and other context).
3. Female-Factor Infertility
This refers to cases in which the primary or sole contributing cause lies in the female partner’s reproductive system.
For example, ovulatory dysfunction (irregular or absent ovulation), diminished ovarian reserve (reduced egg quantity/egg quality), tubal factor (blocked or damaged fallopian tubes), uterine or endometrial factors (uterine fibroids, endometriosis, poor endometrial receptivity).
The clinician (often a reproductive endocrinologist) will assess menstrual cycle regulation, hormone levels (FSH, AMH), ovulation status, ovarian reserve, tubal patency, or uterine anatomy.
Because female fertility declines with age (especially egg quality after age 35–40), the timeframe for intervention may be compressed, meaning earlier work-up and possibly earlier referral for assisted reproductive technologies may be indicated when diminished ovarian reserve or significant structural issues are found.
4. Male-Factor Infertility
This refers to infertility in which the male partner is the primary contributor. Common issues include reduced sperm quality (count, motility, morphology), sperm transport problems, hormonal/andrologic disorders.
For this, evaluation begins with a partner’s semen analysis, hormonal testing (testosterone, FSH, LH), a physical/andrologic exam, and possibly imaging or genetic testing.
Also, management may include lifestyle modifications, medical or surgical treatments (e.g., varicocele repair, hormonal therapy), and assisted reproduction when appropriate.
If the male factor is severe, the timeline for moving to assisted reproductive technologies may be faster rather than prolonged expectant management.
5. Tubal Infertility
This is a specific female-factor category in which the fallopian tubes are blocked, scarred, or damaged, preventing the egg and sperm from meeting or the embryo from reaching the uterus.
It’s often evaluated via imaging (hysterosalpingogram, sonohysterography, or laparoscopy).
If tubal damage is significant (e.g., hydrosalpinx, bilateral obstruction), the timeline for moving to assisted reproduction (such as in vitro fertilization) may be accelerated because natural conception is unlikely.
In some cases, surgical repair may be an option.
6. Combined Infertility
This category applies when both partners (female and male) have contributing fertility-limiting factors.
For example, the female partner may have diminished ovarian reserve or tubal damage, and the male partner may have suboptimal sperm quality.
Because two sets of problems exist, management often needs coordinated care involving both the reproductive endocrinologist and male fertility specialist (andrologist).
Also, the timeline for intervention may be shorter given the combined burden, so clinicians often recommend more proactive assessment and treatment rather than “wait and see.”
7. Unexplained Infertility
This occurs when, after a standard infertility evaluation (including ovulation assessment, ovarian reserve testing, semen analysis, tubal and uterine imaging), no specific cause is identified.
Even though no cause is found, treatment is still possible, but it’s empiric.
Options may include ovulation induction, intrauterine insemination (IUI) timed to the fertile window, or more directly assisted reproductive technologies (ART), depending on age and other risk factors.
Because there is no targetable cause, prognosis depends heavily on age, duration of infertility, and other subtle factors; timing becomes important, especially when the female partner is older.
What Causes Infertility?
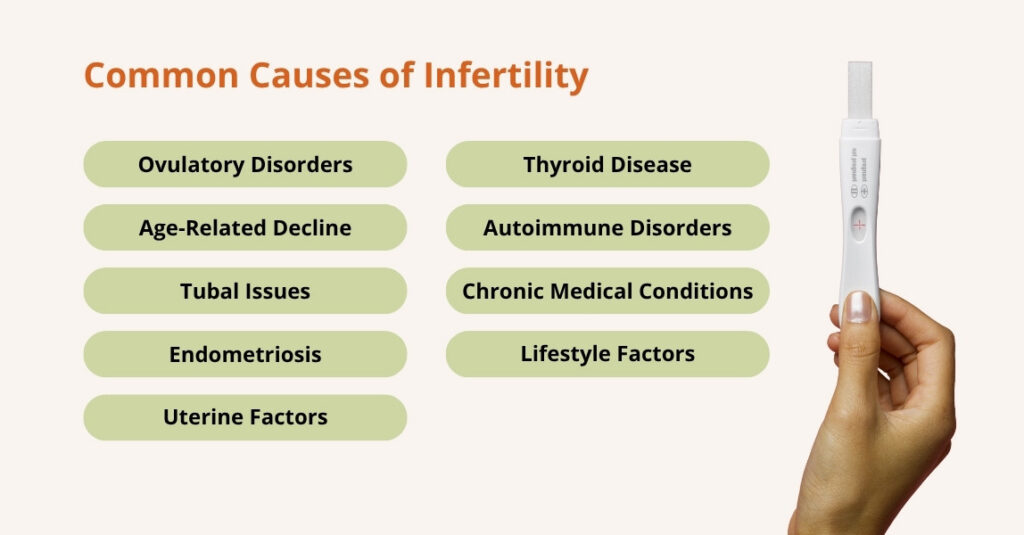
Many underlying medical, lifestyle, and environmental factors can impair egg quality, sperm quality, or the fertilisation/implantation sequence.
The reasons for infertility vary from person to person. Here are the most common causes of infertility in women.
Some reasons for female fertility problems include:
- Ovulatory Disorders
A normal menstrual cycle averages about 28 days; cycles that are fairly regular, roughly every 21 to 35 days, usually indicate that ovulation is occurring. Irregular or infrequent periods often mean ovulation is irregular or absent.
When ovarian function is disrupted, a health-care provider should evaluate possible causes.
Typical tests include follicle-stimulating hormone (FSH), anti-Müllerian hormone (AMH), and antral follicle count (AFC) on pelvic ultrasound.
Common conditions that affect ovarian function
- Polycystic ovary syndrome (PCOS): The most frequent cause of ovulatory infertility. PCOS disrupts the normal hormonal signals that trigger ovulation, causing irregular or absent ovulation and often associated metabolic and androgenic features.
- Diminished ovarian reserve (DOR): Fewer eggs remain in the ovaries than expected for a woman’s age. DOR may be congenital, related to prior surgery or medical treatment, or unexplained; it reduces both the quantity and often the quality of eggs available for fertilization.
- Hypothalamic or pituitary dysfunction: Research shows that problems in the brain’s reproductive control centers (the hypothalamus and pituitary) can alter the release of GnRH, LH, and FSH, impairing follicle development and ovulation.
- Functional hypothalamic amenorrhea (FHA): A reversible condition caused by low body weight, rapid weight loss, excessive exercise, or significant stress. FHA suppresses GnRH secretion and stops or reduces ovulation.
- Primary ovarian insufficiency (POI): Also called premature ovarian failure, POI occurs when the ovaries stop functioning before age 40. It’s characterized by irregular or absent periods, elevated FSH, and low estrogen, and may result in early loss of fertility.
If ovarian dysfunction is suspected, timely evaluation and targeted testing help identify the specific cause and guide management, whether lifestyle changes, medical treatment to restore ovulation, or fertility-preserving or assisted-reproductive options.
- Age-Related Decline
As a woman ages, two key fertility-related processes deteriorate: the number of eggs remaining in her ovaries (often measured as ovarian reserve) and the ability of those eggs to fertilize and develop into healthy embryos (egg quality).
Research shows that age-related changes in oocyte (egg) energy metabolism (for example, reduced ATP production, altered mitochondrial and lipid metabolism) degrade egg quality.
Another study found that the prevalence of Diminished Ovarian Reserve (DOR) increased significantly with age, with more than double the rate in women over 30 compared to those under 30.
Because both quantity and quality decline with age, the “fertile window” shrinks in both monthly opportunities and cumulative chances.
- Tubal Issues
When the tubes are damaged, blocked, scarred, or their epithelial lining is compromised, the egg and sperm cannot meet properly, or the resulting embryo cannot travel safely to the uterus. This condition is known as tubal factor infertility (TFI).
Causes of fallopian tube damage or blockage can include:
- Blockage or scarring: Infections trigger inflammation that leads to adhesions, scar tissue, or complete tubal occlusion, preventing the egg and sperm from meeting.
- Epithelial damage: The ciliated cells of the fallopian tube help transport the fertilised egg into the uterus. Damage to these cells slows or stops embryo transit.
- Ectopic risk: Because the embryo’s path is compromised, implantation may occur in the tube itself rather than the uterus, leading to ectopic pregnancy.
One retrospective cohort of 2,892 women with tubal infertility found that those with prior ectopic pregnancy had worse outcomes in IVF/ICSI cycles.
Because tubal damage is often irreversible, prompt identification can shift management earlier to assisted reproductive technologies (ART) rather than prolonged natural-cycle attempts.
- Endometriosis
Endometriosis is the presence of endometrial-like tissue outside the uterus (for example, on the ovaries, fallopian tubes, or pelvic peritoneum).
This aberrant tissue can cause inflammation, adhesions (scar tissue), hormonal dysregulation, and altered pelvic anatomy. These changes can impact fertility by:
- Impairing ovulation or reducing egg/follicle quality when the ovary is involved (e.g., endometrioma).
- Causing tubal/peritoneal adhesions that interfere with the meeting of egg and sperm or embryo transport.
- Altering the uterine lining (endometrium) so that embryo implantation is less likely.
- Creating a hostile, inflammatory environment in the pelvis may reduce fertility potential.
A study found that women with endometriosis exhibit endometrial changes (hormonal imbalances, immune dysregulation, altered microRNA/gene expression) that reduce the likelihood of successful implantation.
Another research report found that, among women with endometriosis, oxidative stress, dysregulated steroidogenesis (via aromatase P450), and elevated cytokines (IL-6, IL-8, TNF-α) were identified as factors likely impairing follicle/oocyte development and thus fertility.
- Uterine Factors
Uterine-factor infertility refers to conditions in the uterus that interfere with one or more steps of conception, implantation, or maintenance of a pregnancy.
These include anatomical abnormalities and acquired lesions that alter the uterine cavity, lining, or musculature.
A cross-sectional study found a high prevalence of acquired uterine anomalies (polyps, submucosal fibroids) and congenital anomalies (septate, bicornuate uteri) among sub-fertile women.
Because these uterine issues affect the “plumbing and lining” part of the reproductive system, the cavity where the embryo must implant, timely detection and repair can often improve chances of conception.
- Thyroid Disease
According to the American Thyroid Association, one in eight women will develop a thyroid disorder in her lifetime.
Thyroid problems usually fall into two main types:
- Hyperthyroidism (overactive thyroid): The gland makes too much thyroid hormone.
- Hypothyroidism (underactive thyroid): The gland does not produce enough thyroid hormone.
Some people may also develop thyroid nodules, which are small lumps or growths in the thyroid. Most nodules are harmless, but in some cases, they can cause hormonal changes or make swallowing uncomfortable.
Research shows that overt (clinical) hypothyroidism is consistently associated with menstrual irregularities, anovulation, luteal-phase defects, and reduced conception rates. Treating overt hypothyroidism (levothyroxine) typically restores regular cycles and improves chances of conceiving.
Another research from the National Institutes of Health (NIH) also highlights that about 2–4% of women of reproductive age have hypothyroidism.
This condition can interfere with normal ovulation and disrupt menstrual cycles, which may lead to infertility. Hypothyroidism can appear on its own, develop after pregnancy, or occur following treatment for an overactive thyroid. In some cases, it may also be present from birth.
- Autoimmune Disorders
Autoimmune diseases develop when the immune system mistakenly targets the body’s own healthy cells, leading to ongoing inflammation and tissue damage. This heightened immune response can impact fertility in several ways.
A large population-based study analyzed over 568,000 births and discovered that women with untreated infertility were 25% more likely to develop conditions such as lupus, Sjögren’s syndrome, or inflammatory myopathies within nine years after delivery.
Also, the research indicates that infertility itself may act as an early warning sign for underlying autoimmune dysfunction, even when a pregnancy is achieved naturally.
Autoimmune disorders can affect fertility in several ways:
- Hormonal disruptions: Some autoimmune conditions can damage hormone-producing glands, leading to irregular periods and ovulation issues.
- Chronic inflammation: Ongoing inflammation may affect egg quality, embryo development, and the uterus’s ability to accept an embryo.
- Auto-antibodies: In conditions like antiphospholipid syndrome, antibodies can interfere with blood flow to the uterus and placenta, increasing the risk of miscarriage.
- Medication effects: Certain immunosuppressants used to treat autoimmune diseases may temporarily reduce fertility or affect ovarian function.
- Higher miscarriage risk: Women with autoimmune disorders, especially lupus and antiphospholipid syndrome, have a greater chance of pregnancy loss.
Overall, autoimmune activity, inflammation, and treatment effects can all contribute to fertility challenges.
- Chronic Medical Conditions
Long-term illnesses such as diabetes, hypertension, autoimmune disorders, kidney disease, and untreated thyroid problems can disrupt the delicate hormonal balance needed for ovulation and healthy menstrual cycles.
These conditions may also affect blood flow to reproductive organs, increase inflammation, or lead to complications like irregular periods, poor egg quality, or difficulty maintaining a pregnancy.
For example, research shows that chronic metabolic disorders such as obesity and metabolic syndrome impair fertility by disrupting the hypothalamic–pituitary–ovarian (HPO) axis, lowering oocyte quality, and reducing implantation and live-birth rates; multiple recent reviews document these mechanisms and worse assisted reproduction outcomes in obese women.
Another research indicates that decreased ovarian reserve, altered ovarian function, and worse clinical pregnancy rates in women with diabetes.
- Lifestyle Factors
Unhealthy habits such as smoking, excessive alcohol use, poor diet, and lack of exercise can disrupt the hormonal balance required for ovulation and regular menstrual cycles.
Moreover, exposure to environmental toxins, like pesticides, plastics (BPA), and certain chemicals, may also damage eggs and sperm or affect implantation.
Plus, poor sleep, chronic dehydration, and overuse of caffeine further strain the body’s hormonal regulation.
What are the Signs of Infertility?
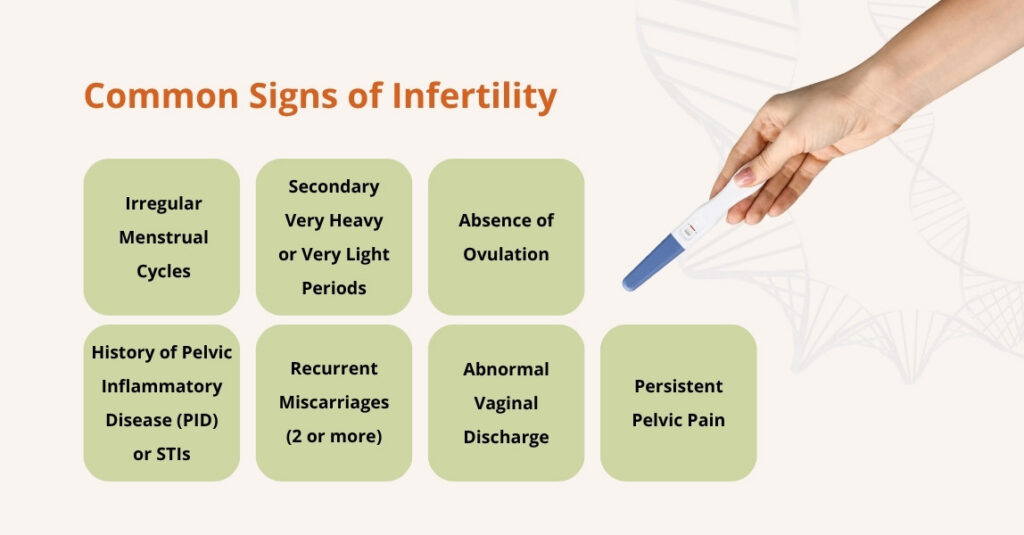
Infertility in people who menstruate is often first suspected from objective clues in the reproductive history, physical exam, or simple tests.
Many of these signs point to hormonal or structural problems that can impair ovulation, egg quality, tubal function, or uterine receptivity.
The common signs of infertility include:
- Irregular menstrual cycles: Cycles shorter than 21 days, longer than 35 days, or unpredictable, often a sign of ovulatory problems like PCOS or hormonal imbalance.
- Very heavy or very light periods: Abnormal flow can signal fibroids, polyps, hormonal disorders, or uterine lining problems that affect implantation.
- Absence of ovulation: No ovulation confirmed by tests (like low mid-luteal progesterone). Seen in PCOS, thyroid issues, hyperprolactinemia, or POI.
- History of pelvic inflammatory disease (PID) or STIs: Documented infections such as chlamydia or gonorrhea increase the risk of tubal scarring and blocked fallopian tubes.
- Recurrent miscarriages (2 or more): Repeated pregnancy loss may indicate uterine abnormalities, genetic issues, autoimmune disorders, or hormonal imbalance.
- Abnormal vaginal discharge (infection-related): Clinically confirmed infections can travel upward and damage the tubes, affecting fertility.
- Persistent pelvic pain: Exam-related or recorded chronic pelvic pain may be a sign of endometriosis or pelvic adhesions that interfere with conception.
What are the Symptoms of Infertility
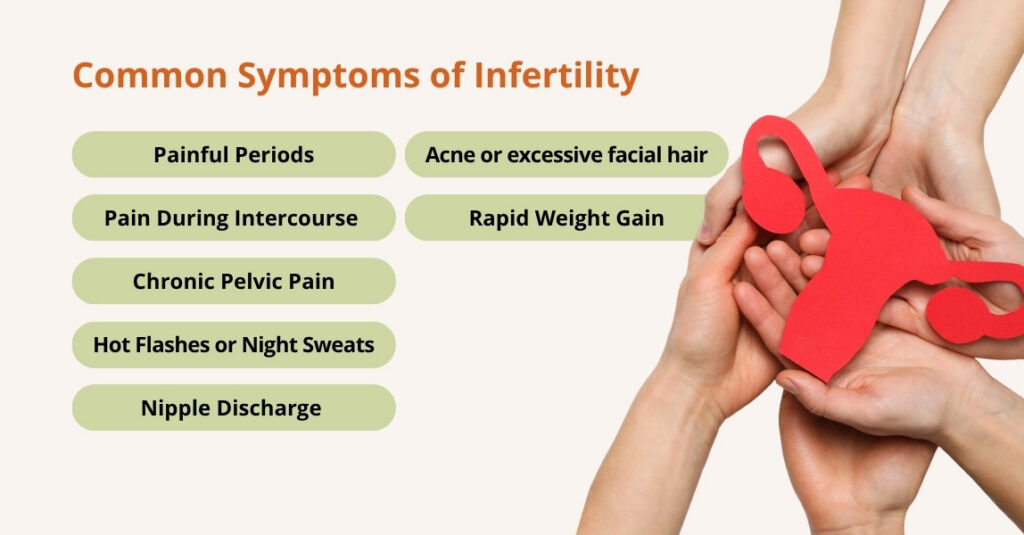
While infertility itself often has no symptoms, many women experience physical changes that point to an underlying condition affecting their reproductive health.
Common symptoms linked to infertility include:
- Painful periods (dysmenorrhea): Severe cramping may indicate endometriosis or pelvic inflammation.
- Pain during intercourse (dyspareunia): Often linked to endometriosis, pelvic adhesions, or chronic inflammation.
- Chronic pelvic pain: Persistent pain outside menstruation may reflect endometriosis, fibroids, or pelvic scarring.
- Hot flashes or night sweats: A sign of low estrogen and possible premature ovarian insufficiency (POI).
- Nipple discharge (galactorrhea): Can indicate hyperprolactinemia, which disrupts ovulation.
- Rapid weight gain: Frequently associated with insulin resistance or hormonal imbalance, especially in PCOS.
- Acne or excessive facial hair (hirsutism): Signs of androgen excess are often seen in PCOS and other ovulatory disorders.
How Is Infertility Diagnosed?
No single test can detect every cause of infertility, and many tests miss mild problems.
A comprehensive approach typically includes:
Detailed Medical History and Physical Exam
Your clinician reviews your menstrual cycle, past pregnancies, infections, surgeries, medications, lifestyle factors, and overall health.
A pelvic exam checks for fibroids, ovarian masses, or signs of endometriosis. This guides which tests come next.
Basic Ovulation Testing (Is ovulation occurring?)
Home ovulation kits detect the LH surge and help time intercourse.
Also, a mid-luteal progesterone test is performed ~7 days before your period to confirm ovulation. Low levels suggest absent or irregular ovulation.
Ovarian-Reserve Testing (How many eggs remain/ovarian activity)
It typically includes three key measures:
- AMH (anti-Müllerian hormone): A blood test that can be done any time in the cycle and provides an estimate of ovarian reserve.
- FSH and estradiol: Usually measured on cycle day 2–4; an elevated FSH or abnormal estradiol can indicate reduced reserve.
- Antral follicle count (AFC): A transvaginal ultrasound performed early in the cycle counts small follicles and gives a visual estimate of ovarian reserve.
Transvaginal ultrasound (TVUS) (structural and functional imaging)
A transvaginal ultrasound evaluates the uterus and ovaries: it detects fibroids, ovarian cysts or endometriomas, and helps assess the antral follicle count.
It’s a routine, non-invasive test used throughout the diagnostic workup.
Tests of Tubal Patency
To check whether eggs and sperm meet, the following tests are done:
- Hysterosalpingography (HSG): X-ray with contrast to see if the fallopian tubes are open.
- Saline infusion sonohysterogram (SIS): ultrasound with saline to detect polyps, fibroids, or adhesions in the uterine cavity.
Diagnostic Laparoscopy (Selected cases)
A laparoscopy is a minimally invasive surgery (small incisions, camera into the pelvis) reserved for specific indications: suspected endometriosis not visible on imaging, persistent pelvic pain, or unclear tubal disease after HSG/other tests.
It can both diagnose and, in some cases, treat adhesions or endometriosis.
Remember, the testing protocols vary between providers, so it is reasonable to seek a second opinion if you’re unsure about results or next steps.
Infertility Treatment Options: From Least Invasive to Most Advanced
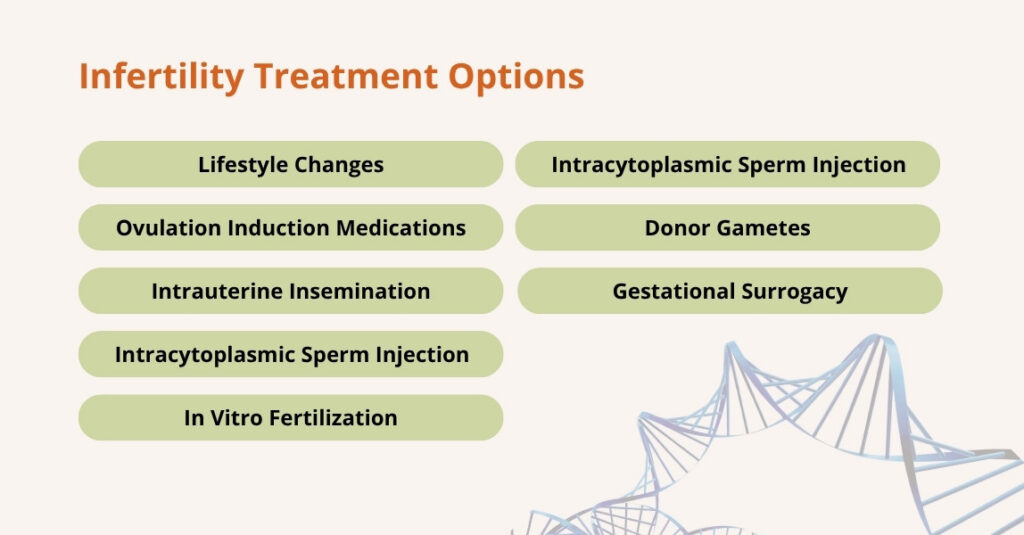
Infertility treatments vary in complexity and invasiveness, ranging from lifestyle changes to advanced assisted reproductive technologies (ART). Also, they are tailored to age, diagnosis, and reproductive goals.
Here are some of the most commonly used infertility treatment options:
Lifestyle Changes
Optimizing overall health can naturally improve fertility. This includes achieving a healthy weight, eating a balanced diet, quitting smoking, limiting alcohol, managing stress, and avoiding endocrine-disrupting chemicals.
Even modest lifestyle adjustments can improve ovulation, egg quality, sperm quality, and endometrial receptivity.
Ovulation Induction Medications
For women with ovulatory dysfunction (such as PCOS or hormonal imbalance), medications stimulate ovulation:
- Clomiphene citrate: Oral medication that induces ovulation.
- Letrozole: An aromatase inhibitor often preferred for women with PCOS.
- Gonadotropins: Injectable hormones for more controlled ovarian stimulation.
Hormonal regulation may also include correcting thyroid, prolactin, or luteal-phase deficiencies.
Intrauterine Insemination (IUI)
IUI involves placing washed sperm directly into the uterus around the conception window to increase the chances of fertilization.
Often combined with ovulation induction. Suitable for mild male factor infertility, unexplained infertility, or cervical issues.
In Vitro Fertilization (IVF)
IVF is an ART procedure where eggs are retrieved from the ovaries, fertilized with sperm in a lab, and the resulting embryos are cultured to the blastocyst stage for transfer.
Embryo grading helps select the best embryos for transfer, maximizing success rates. IVF is used for tubal ligation factor, severe male infertility, or when IUI has failed.
Intracytoplasmic Sperm Injection (ICSI)
A specialized form of IVF where a single sperm is injected directly into an egg. Often used for severe male infertility, low sperm count, poor motility, or previous fertilization failure in IVF.
Donor Gametes
When a woman’s eggs are of poor quality, or a man has no viable sperm, donor eggs or sperm can be used. This allows fertilization with donor genetic material.
This is often recommended for women over 40 or for couples where male infertility is severe. Donor eggs have a higher success rate in older women.
Gestational Surrogacy
Gestational surrogacy involves another woman carrying a pregnancy for a couple who cannot conceive or carry a pregnancy themselves. The embryo is created through IVF using the eggs and sperm from the intended parents or donors.
It is typically used when a woman cannot carry a pregnancy due to health conditions or failed IVF cycles.
Fertility Preservation (Egg/Embryo Freezing)
Fertility preservation includes freezing eggs or embryos for future use. This is often done by women who wish to delay childbearing for personal or medical reasons, such as cancer treatment.
Common for women over 35 who want to delay childbearing, or for those facing medical treatments that may affect fertility.
However, for men, sperm freezing is an option before undergoing treatments like chemotherapy.
Choosing the right treatment requires a personalized evaluation by a reproductive endocrinologist or fertility specialist, taking into account age, diagnosis, and prior response to therapy.
Complications of Infertility Treatment
Infertility treatments, especially those involving hormonal stimulation or assisted reproduction, carry some risks, though serious problems are relatively rare.
Here are some complications of infertility treatment:
Ovarian Hyperstimulation Syndrome (OHSS)
OHSS occurs when the ovaries over-respond to stimulation, causing fluid leakage, ovarian swelling, and sometimes more severe effects.
A recent large review estimated that moderate to severe OHSS affects 1–5% of IVF cycles. Severe OHSS can lead to complications such as hemoconcentration, clotting risk, and more.
Multiple Pregnancy Risk
Fertility treatments (especially when more than one embryo is transferred, or with strong ovulation stimulation) increase the likelihood of twins or higher-order multiples.
Also, multiple gestations are a major contributor to pregnancy complications after fertility treatment. Studies show that many of the excess risks (preterm birth, cesarean section, preeclampsia) are mediated by having multiples.
Ectopic Pregnancy
Although relatively uncommon, ectopic pregnancy (when an embryo implants outside the uterus) can occur following fertility treatment.
Research shows that ectopic pregnancies have been observed as one of the more serious adverse events, especially in protocols involving embryo transfer.
Emotional Stress, Anxiety, Depression
The emotional toll of infertility treatments can be significant, leading to increased stress, anxiety, and depression.
The uncertainty of treatment outcomes, coupled with hormonal changes, can exacerbate these feelings.
For this, support from counselors, support groups, and a strong partner relationship can help alleviate emotional distress.
Procedure-Related Discomfort
Some infertility treatments, particularly egg retrieval and sperm collection procedures, may cause temporary discomfort or pain.
These procedures are generally quick and performed under sedation or local anesthesia, ensuring patient comfort.
Financial and Insurance Considerations
Infertility treatments can be expensive, and not all insurance plans cover the full cost.
This financial burden can add stress to the process, but many fertility clinics offer payment plans, and some regions have specific fertility treatment insurance coverage.
Medication Side Effects
Fertility drugs (gonadotropins, hCG trigger, etc.) can cause side effects like bloating, nausea, mood changes, and fluid shifts.
Because some protocols involve high doses of hormones, the body’s response can be quite variable, which is why close monitoring is essential.
While there are potential complications associated with infertility treatments, most are rare and manageable with appropriate medical supervision.
To address these, open communication with healthcare providers and proper monitoring significantly reduce the chances of severe complications.
How to Prevent Infertility?
While not all cases of infertility are preventable, many risk factors are modifiable, and taking proactive steps to address these factors can improve your chances of maintaining fertility.
Here are some practical ways to reduce your risk:
- Maintain a Healthy BMI: A healthy weight supports regular menstrual cycles and ovulation.
- Quit Smoking: Smoking affects egg quality in women and sperm in men, reducing fertility.
- Limit Alcohol Intake: Excess alcohol can disrupt hormone production and ovulation.
- Use STI Protection: Condoms and regular screenings can prevent infections that damage reproductive organs.
- Treat Infections Promptly: Prompt treatment of infections such as pelvic inflammatory disease (PID) prevents fertility issues.
- Manage Thyroid Disease: Regular monitoring and treatment of thyroid issues support fertility.
- Control Chronic Conditions: Managing diabetes and autoimmune disorders reduces their impact on fertility.
- Reduce Toxin Exposure: Limiting exposure to BPA and pesticides protects reproductive health.
- Get Regular Well-Woman Exams: Regular exams help detect fertility issues early.
- Track Menstrual Cycles: Monitoring your cycle helps identify irregularities that may affect fertility.
By taking these steps, individuals can improve their reproductive health and increase their chances of conception.
Frequently Asked Questions (FAQs)
Why am I not getting pregnant?
Not getting pregnant can be frustrating, but it is often related to a combination of factors involving both partners. Several factors can affect fertility:
- Ovulation Issues: Irregular ovulation can prevent conception. Tracking ovulation can help identify this issue.
- Male-Factor Infertility: Low sperm count or poor motility can impact fertility. A semen analysis can identify sperm issues.
- Age: As you age, egg quality and quantity decline, reducing the chances of pregnancy.
- Timing: Conception is most likely when intercourse happens close to ovulation.
- Underlying Conditions: Conditions like thyroid disorders or diabetes can affect fertility.
How to know if you’re infertile?
You may consider a fertility evaluation if you haven’t conceived after 12 months of trying (<35 years) or 6 months (≥35 years). Earlier assessment is recommended for signs like irregular periods, missed ovulation (anovulation), recurrent miscarriages, or known reproductive conditions. Tests often include cycle monitoring, ovulation tracking, and AMH testing to assess ovarian reserve and guide next steps.
How common is infertility?
Infertility affects a significant number of couples in the U.S. According to the CDC, about 19% of married women aged 15–49 with no prior births are unable to get pregnant after one year of trying. Delays in childbearing (women starting families later) and demographic shifts contribute to this trend.
Is infertility genetic?
Yes, genetics can play a role in certain infertility conditions. Some women may inherit risks for endometriosis, premature ovarian insufficiency (POI), or polycystic ovary syndrome (PCOS), while men can inherit Y-chromosome deletions or Klinefelter syndrome, affecting sperm production. Therefore, a family history of reproductive issues can signal a higher risk. Couples concerned about hereditary infertility may benefit from genetic counseling to understand risks and testing options.
Can infertility be cured?
Some infertility causes are treatable; for example, hormonal imbalances can be managed with medications, ovulation issues may improve with lifestyle changes, and structural problems like fibroids or tubal blockages can sometimes be corrected surgically. Other cases may not be fully “curable” but can be managed effectively with assisted reproductive technologies (ART) such as IVF. Success depends on the underlying cause, age, and overall reproductive health.
Conclusion
Infertility is a common medical condition, affecting nearly 1 in 5 women of reproductive age in the U.S., and often involves factors from both partners.
Causes range from ovulation disorders, tubal or uterine issues, and age-related egg decline to male-factor infertility, including low sperm count or genetic conditions.
Many signs, such as irregular cycles, recurrent miscarriages, or difficulty conceiving despite regular intercourse, can signal the need for evaluation. Plus, symptoms like painful periods or hormonal changes may indicate underlying disorders.
The good news is that most infertility causes are treatable or manageable. Lifestyle changes, ovulation induction, hormonal therapy, surgical correction, or advanced ART procedures like IVF and ICSI can significantly improve the chance of conception.
While the journey can be emotionally challenging, understanding the causes, monitoring cycles, and accessing appropriate care empowers couples.
Infertility is not a reflection of personal failure, and with timely support and evidence-based treatment, many individuals and couples achieve successful pregnancy outcomes. Your fertility matters, and help is available.

Leave a Reply