A swollen knee, often called knee effusion, means extra fluid has collected inside the joint or in the tissues that surround it.
Because the knee is a large hinge joint that supports your body weight and allows a wide range of motion, even mild swelling can be painful and make walking or bending difficult.
Swelling may occur suddenly after a traumatic injury, or it can develop gradually as the result of chronic inflammation or degenerative disease.
Although swelling itself is not a diagnosis, it is an important warning sign that something else is wrong. Causes range from minor sprains and ligament tears to more serious problems such as infections or autoimmune conditions.
In the United States, knee injuries account for over half a million emergency department visits each year, and the lifetime prevalence of knee swelling is estimated at 27%. These numbers show how common knee problems are and why prompt attention matters.
This guide walks through what a swollen knee is, its common causes and risk factors, symptoms to watch for, possible complications, how clinicians diagnose it, evidence-based treatment options, and practical steps you can take to reduce the risk of recurrence.
What is a Swollen Knee?
Knee swelling happens when extra fluid builds up in or around the knee joint. The knee connects your thigh bone (femur) to your shin bone (tibia) and kneecap (patella).
It’s the largest joint in your body, supported by cartilage, muscles, ligaments, and nerves. Because so many structures work together, anything that irritates or injures the knee can lead to swelling.
Swelling can occur after an injury or develop due to an underlying health condition affecting the tissues around the joint.
When your knee is swollen, you may also notice:
- Knee pain
- Stiffness or a tight feeling
- Redness or discoloration
- Warmth or heat around the joint
Most mild cases can be managed at home with rest, ice, elevation, and over-the-counter (OTC) medicine.
However, you should see a healthcare provider if the swelling follows a fall or sports injury, doesn’t improve after a few days, causes severe pain, or makes it hard to move your knee.
What Causes a Swollen Knee?

Since swelling is a symptom, not a condition in itself, it can result from a wide range of underlying conditions.
Here are the key causes of a swollen knee:
1. Traumatic Injuries
Trauma is a leading cause of acute knee swelling. Injuries often occur during sports, falls, or motor vehicle collisions. When soft tissues or bone structures in the knee are damaged, blood vessels rupture, and synovial membrane irritation leads to effusion.
These include:
- Ligament Injuries
Ligament tears, especially of the anterior cruciate ligament (ACL), are a leading cause of acute swelling. ACL injuries often happen with a sudden pivot or landing, and people commonly report an audible “pop,” sharp pain, rapid swelling within hours, and a feeling that the knee will give way.
A systematic review indicates that ACL tears often accompany bone bruises, meniscus damage, or cartilage injury, all of which can lead to bleeding or joint fluid build-up (hemarthrosis), a common cause of swelling.
Whereas posterior cruciate ligament (PCL) injuries are less common but produce similar symptoms: pain, rapid swelling, stiffness, and difficulty walking.
- Meniscal Tears
The menisci are crescent-shaped cartilage cushions between the femur and tibia.
A twisting injury can tear a meniscus, causing pain, stiffness, swelling, difficulty fully straightening the knee, and occasional locking or catching.
- Fractures
Breaks involving the patella, distal femur, or proximal tibia can lead to substantial swelling because bone bleeding often fills the joint space (hemarthrosis).
If the patient cannot bear weight or the leg looks deformed, prompt X-rays or CT scans are essential.
- Dislocations
Patellar dislocation, when the kneecap slips out of its groove, is relatively common and causes sudden pain, visible deformity, and swelling.
2. Inflammatory Conditions
Inflammatory arthritides can provoke episodic or chronic knee swelling. They result from autoimmune processes or crystal deposition within the synovium.
- Rheumatoid Arthritis (RA)
Rheumatoid arthritis is a systemic autoimmune disease that causes chronic inflammation of the synovial lining. Although it usually starts in the small joints of the hands and feet, larger joints, including the knee, are frequently affected.
Thus, persistent synovitis causes swelling, warmth, pain, stiffness, and gradual joint damage.
- Gout and Pseudogout (Crystal Arthropathies)
Gout is caused by the deposition of monosodium urate crystals in joints due to hyperuricemia. While the big toe is the classic site, gout can also affect the knees, ankles, and wrists.
Whereas Pseudogout, also called calcium pyrophosphate deposition disease (CPPD), involves deposition of calcium pyrophosphate crystals in articular cartilage and soft tissues. Flares mimic gout but are more likely to involve the knees and wrists.
- Septic Arthritis
Septic arthritis is an infection of the joint space, most commonly caused by bacteria. Pathogens enter the knee through hematogenous spread, direct inoculation (trauma or surgery), or extension from osteomyelitis.
Research shows that if a knee injury with hemarthrosis is not treated promptly or properly, patients face a significantly higher risk of developing knee osteoarthritis over the next 10 to 12 years.
The knee becomes extremely painful, swollen, warm, and difficult to move, and patients often have fever or systemic signs of infection.
- Viral Arthritis
Acute viral infections can cause transient arthritis due to immune activation and direct viral invasion. Common culprits include parvovirus B19, hepatitis B and C, Epstein–Barr virus, chikungunya, rubella, and arthropod‑borne viruses.
Viral arthritis is acute, generalized inflammation of joints triggered by a broad range of viruses; it presents with joint pain, swelling, fever, rash, and fatigue, and usually resolves spontaneously once the infection is cleared.
3. Degenerative Conditions
Degenerative processes gradually erode joint structures, leading to chronic swelling.
- Osteoarthritis
Osteoarthritis is the most common cause of chronic knee swelling. It develops as cartilage breaks down and the joint becomes inflamed.
OA affects over 32 million U.S. adults and is most common in people aged 55–64, though many younger adults are also affected.
Typical symptoms include gradual pain that worsens with activity, stiffness after rest, creaking sensations, and occasional fluid buildup.
- Patellofemoral Pain Syndrome (PFPS)
Often called “runner’s knee,” PFPS causes pain at the front of the knee due to irritation in the patellofemoral joint.
People may notice a dull ache, discomfort with running or climbing stairs, pain after sitting, and sometimes mild swelling after activity. Also, overuse, muscle imbalance, poor alignment, and improper footwear are common triggers.
- Bursitis
The knee contains several small bursae that reduce friction. Repetitive kneeling, irritation, or infection can inflame these sacs, leading to prepatellar or infrapatellar bursitis. Symptoms include localized swelling, tenderness, and warmth.
4. Infectious Conditions
In addition to septic arthritis and bursitis, infections caused by atypical organisms, such as fungi or mycobacteria, can cause joint swelling, especially in people with weakened immune systems.
These infections may develop more slowly or present with less typical symptoms, so prompt joint aspiration, culture, and targeted (culture-directed) treatment are essential to prevent ongoing damage.
5. Other Systemic Causes
Some systemic diseases can lead to knee swelling through immune or metabolic processes.
- Systemic Lupus Erythematosus (SLE)
SLE is an autoimmune condition that can affect multiple organs, including the joints. Around 95% of patients experience joint pain or arthritis, often involving large joints like the knees.
- Lyme Disease
Lyme arthritis is caused by infection with Borrelia burgdorferi, transmitted via tick bites. Untreated Lyme disease often leads to recurrent knee swelling, with about 60% of cases developing arthritis.
Most patients respond to a 30-day course of oral antibiotics like doxycycline or amoxicillin, while persistent cases may require intravenous antibiotics.
- Hyperuricemia (Gout)
High uric acid levels, whether from genetics, metabolic syndrome, or reduced kidney excretion, can trigger gouty flares, including in the knee.
What are the Symptoms of a Swollen Knee?

The signs of a swollen knee can vary depending on the cause, but common symptoms include:
- Visible swelling around the kneecap or general enlargement of the joint.
- Tightness or stiffness, often with a feeling of fullness or pressure.
- Pain, ranging from mild discomfort to severe throbbing, especially when bearing weight or moving the knee.
- Warmth and redness if inflammation or infection is present.
- Limited range of motion, making it difficult to fully bend or straighten the knee.
- Instability or locking, particularly with mechanical injuries like ligament or meniscus tears.
- Systemic symptoms such as fever, chills, or fatigue, in cases of infection or autoimmune disease.
Because swelling can hide underlying injuries or joint damage, any persistent or severe knee effusion should be evaluated by a healthcare professional.
What are the Common Risk Factors of a Swollen Knee?
Certain factors increase the likelihood of knee swelling. These include:
- Age: Older adults are more susceptible to degenerative conditions, such as knee osteoarthritis.
- Previous Knee Injuries: A history of fractures, ligament tears, or meniscal injuries predisposes to future swelling due to residual instability and cartilage damage.
- Obesity: Excess body weight increases mechanical load on the knee, accelerating cartilage wear and predisposing to osteoarthritis.
- Physical Activity: High‑impact sports or occupations that involve repetitive kneeling, squatting, or twisting increase injury risk. Conversely, insufficient physical activity weakens the muscles that support the knee.
- Medical Conditions: Rheumatoid arthritis, gout, pseudogout, lupus, psoriasis, and metabolic diseases can cause recurrent joint inflammation.
- Genetics: Family history of osteoarthritis or connective tissue disorders may increase susceptibility.
What are the Complications of a Swollen Knee?
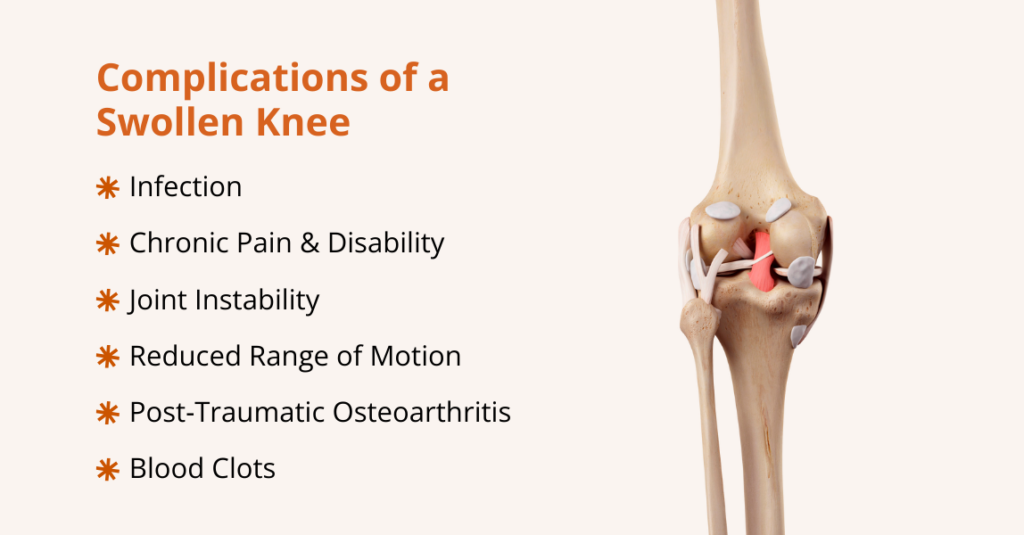
Untreated or chronic knee effusion can lead to several complications:
- Infection: Delayed diagnosis of septic arthritis allows bacteria to destroy cartilage and enter the bloodstream, potentially causing sepsis.
- Chronic Pain and Disability: Persistent swelling from osteoarthritis or inflammatory arthritis results in ongoing pain, reduced mobility, and diminished quality of life.
- Joint Instability: Ligament injuries that cause effusion may lead to ongoing instability and increased risk of recurrent injuries.
- Reduced Range of Motion: Effusion and synovial thickening limit joint motion, leading to contractures.
- Post‑Traumatic Osteoarthritis: Long‑standing swelling after trauma accelerates cartilage degeneration and can lead to secondary osteoarthritis.
- Blood Clots (Deep Vein Thrombosis): Immobilization and inflammatory states increase the risk of venous thromboembolism.
How to Diagnose a Swollen Knee?
You can often tell a knee is swollen by comparing it to the other side: a swollen knee looks puffy or larger, the skin may appear shiny or stretched, and the joint can feel warm, tight, or painful, especially when you try to bend or straighten the leg.
You may also notice uneven contours, reduced motion, or a sense of pressure or fullness inside the joint.
Healthcare providers usually follow a stepwise approach to diagnose a swollen knee:
1. Clinical Evaluation
Diagnosing a swollen knee starts with a detailed history and physical exam:
- History: Clinicians ask about the onset (sudden or gradual), prior injuries or infections, activity level, medications, comorbidities, and symptoms such as fever or rash.
- Inspection & Palpation: The knee is checked for asymmetry, bruising, deformity, warmth, tenderness, effusion, and patellar mobility. Joint line tenderness is also assessed.
- Range of Motion (ROM) & Special Tests: Active and passive ROM are compared to the other knee. Specific tests, such as the Lachman (ACL), posterior drawer (PCL), McMurray (meniscus), and patellar apprehension tests, help pinpoint injuries.
2. Imaging Studies
Imaging helps confirm diagnoses and assess structural damage:
- X‑Ray: First‑line imaging to evaluate fractures, degenerative changes, and patellar alignment.
- Ultrasound: Useful for detecting joint effusions, guiding aspirations, and evaluating bursitis or soft tissue injuries.
- Magnetic Resonance Imaging (MRI): Gold standard for visualizing ligaments, menisci, cartilage, and bone marrow lesions. MRI can detect occult fractures, bone contusions, and synovial proliferation.
- Computed Tomography (CT): Provides detailed bone images for complex fractures or preoperative planning.
3. Arthrocentesis (Joint Aspiration)
When the etiology is unclear or infection is suspected, joint aspiration is invaluable. Under sterile technique, a needle is inserted into the joint to withdraw fluid.
The fluid is analyzed for color, clarity, viscosity, white cell count, crystals, and microorganisms. This distinguishes inflammatory from non‑inflammatory effusions, identifies septic arthritis, and diagnoses gout or pseudogout.
Therapeutically, removing fluid can relieve pressure and improve mobility. Intra‑articular corticosteroid injection may be performed concurrently for inflammatory conditions.
4. Laboratory Tests
The following blood tests can aid in diagnosis:
- Complete blood count (CBC) and C‑reactive protein (CRP)/Erythrocyte sedimentation rate (ESR)
- Uric Acid Test
- Rheumatoid Factor (RF) and Anti‑CCP
- Antinuclear Antibody (ANA)
- Culture and Gram Stain
Swollen Knee Treatment Options
Treatment for a swollen knee depends on the underlying cause, the severity and duration of symptoms, and other factors.
Mild or short-term swelling from minor injuries can often be managed at home. Still, persistent, recurrent, or severe swelling may require medical evaluation and targeted interventions, or surgical options may be considered to address the issue.
At home
For many minor injuries and mild inflammation, conservative management suffices:
- Rest: Avoid activities that worsen pain; short periods of limited weight‑bearing and the use of crutches may be necessary.
- Ice: Apply cold packs for 15–20 minutes every few hours during the first 48–72 hours to reduce swelling.
- Compression: Elastic bandages or sleeves help limit swelling; ensure they are not too tight.
- Elevation: Keeping the knee above heart level assists venous return and reduces edema.
- Non‑steroidal Anti‑Inflammatory Drugs (NSAIDs): Ibuprofen or naproxen relieve pain and inflammation. However, caution is needed in patients with kidney disease or gastrointestinal ulcers.
- Activity Modification and Bracing: Temporarily avoiding high‑impact activities and using a knee brace can stabilize the joint during healing.
- Physical Therapy: A structured rehabilitation program restores range of motion, strengthens surrounding muscles, improves balance, and reduces the risk of recurrence.
Minimally Invasive Procedures
When conservative measures fail, minimally invasive interventions may be considered:
- Genicular Artery Embolization (GAE): It is a minimally invasive procedure performed by a board-certified interventional radiologist to treat chronic knee pain, often due to osteoarthritis, by targeting the small blood vessels (genicular arteries) that supply the inflamed synovium.
- Corticosteroid Injections: Intra‑articular corticosteroids reduce inflammation and provide rapid symptom relief for conditions like rheumatoid arthritis, gout, or OA flares. However, repeated injections may damage cartilage or increase the risk of infection.
- Platelet‑Rich Plasma (PRP) Injections: PRP, derived from the patient’s own blood, contains growth factors that may promote tissue healing. Emerging evidence suggests benefit in early osteoarthritis and chronic tendon injuries.
- Hyaluronic Acid (Viscosupplementation): Injecting hyaluronic acid aims to improve joint lubrication in osteoarthritis. Some patients experience modest pain relief lasting several months.
- Cryoablation: Freezing sensory nerves can provide longer‑lasting pain relief in chronic conditions. It may be considered in select patients after other therapies fail.
Surgical Management
Surgery is reserved for severe injuries or advanced disease:
- Arthroscopic Surgery: Minimally invasive arthroscopy allows surgeons to repair or remove torn meniscal fragments, trim damaged cartilage, reconstruct ligaments (ACL or PCL), or remove loose bodies.
- Open or Arthroscopic Fracture Fixation: Stabilizes displaced fractures to facilitate healing and early mobilization.
- Synovectomy: Surgical removal of inflamed synovial tissue may be performed in refractory rheumatoid arthritis or pigmented villonodular synovitis.
- Total Knee Replacement (Arthroplasty): Replaces the diseased joint surfaces with artificial implants. This procedure is considered when pain and swelling severely limit function and conservative treatments fail.
Postoperative Care and Rehabilitation
Following surgery, appropriate postoperative care is essential:
- Pain Management: Multimodal analgesia (NSAIDs, acetaminophen, opioids, nerve blocks) and cryotherapy help control pain.
- Early Mobilization: Guided by surgeons and physical therapists, patients begin gentle ROM exercises and weight‑bearing as tolerated to prevent stiffness and blood clots.
- Physiotherapy: Progressive strengthening and endurance exercises restore function and reduce the risk of complications.
How to Prevent a Swollen Knee?
Although not all causes of knee swelling are preventable, adopting healthy habits reduces the risk:
- Protective Equipment: Use knee pads during sports and occupations that involve frequent kneeling or contact.
- Weight Management: Maintaining a healthy body weight reduces mechanical stress and lowers the risk of osteoarthritis.
- Strength Training: Strengthening quadriceps, hamstrings, gluteal, and core muscles enhances joint stability.
- Low‑Impact Exercise: Incorporate activities like swimming, cycling, or elliptical training that minimize joint stress while maintaining cardiovascular fitness.
- Proper Technique: Learn proper form for sports and weight lifting to avoid sudden twisting or hyperextension injuries.
- Stretching: Regular stretching of the quadriceps, hamstrings, and calf muscles maintains flexibility and reduces strain on the knee.
- Early Management of Chronic Diseases: Prompt treatment of autoimmune diseases, metabolic syndrome, and gout reduces flare‑ups and joint damage.
- Regular Monitoring: Individuals at high risk (athletes, older adults, and those with prior knee injuries) should undergo periodic medical evaluations to detect early changes.
Frequently Asked Questions (FAQs)
Can a swollen knee be dangerous?
Yes. While many causes are benign, rapid swelling accompanied by fever, severe pain, or inability to bear weight may signal a fracture, ligament tear, or septic arthritis and should prompt immediate medical attention. Delay in treatment increases the risk of permanent damage and systemic infection.
What can I do for a swollen knee at home?
Follow the RICE protocol: rest, ice, compression, and elevation. Use NSAIDs for pain if safe. Avoid activities that exacerbate symptoms. However, if swelling lasts more than a few days or recurs frequently, see a healthcare provider.
How long does it take for knee swelling to go down?
The time it takes for knee swelling to go down depends on the cause and severity of the injury or condition. Mild swelling from minor strains or overuse may improve within a few days to a week with rest, ice, compression, and elevation. Whereas swelling from more significant injuries, such as ligament tears, fractures, or hemarthrosis, can take several weeks to months to resolve, especially if rehabilitation or medical treatment is required. Chronic conditions such as arthritis or gout may cause intermittent swelling that persists or recurs over time and often requires ongoing management to control inflammation.
When should I worry about a swollen knee?
You should worry about a swollen knee if it is sudden, severe, or persistent, or comes with warning signs. Seek urgent care if you have rapid swelling, inability to bear weight, severe pain, deformity, redness, warmth, fever, or numbness. See a doctor soon if swelling doesn’t improve after a few days, recurs, causes locking or instability, or is accompanied by systemic symptoms. Early evaluation helps prevent joint damage and identify serious causes such as infection, fractures, or ligament injuries.
What happens if a swollen knee is left untreated?
Ignoring persistent swelling can lead to complications such as cartilage degeneration, chronic instability, decreased range of motion, and, in cases of infection, joint destruction and sepsis.
What does a swollen knee indicate?
A swollen knee indicates that there is excess fluid in or around the joint, which is usually a sign of an underlying problem rather than a condition on its own. It can result from injuries (ligament tears, meniscus tears, fractures), degenerative changes (osteoarthritis), infections (septic arthritis, bursitis), inflammatory or autoimmune diseases (rheumatoid arthritis, lupus), or crystal deposits (gout, pseudogout). The swelling reflects inflammation, bleeding, or fluid buildup in the knee, and its cause determines the severity, associated symptoms, and treatment required.
What does a swollen knee look like?
A swollen knee usually appears larger or puffier than the other knee. The skin may look shiny, stretched, or tight, and the joint can feel warm to the touch. Swelling may cause uneven contours around the kneecap or along the joint line. In some cases, redness or bruising is visible, and the knee may appear stiff or slightly deformed. Swelling can make it difficult to fully bend or straighten the leg.
Conclusion
A swollen knee is a symptom with many possible causes, ranging from traumatic injuries such as ACL or meniscus tears, fractures, and patellar dislocations, to inflammatory conditions such as rheumatoid arthritis, gout, and pseudogout, to degenerative osteoarthritis in older adults.
Serious infections like septic arthritis and bursitis require prompt recognition and treatment, while less common systemic causes include SLE, Lyme disease, and metabolic disorders.
Early diagnosis and intervention are crucial to prevent complications, reduce pain, and preserve joint function. Therefore, proper evaluation, including history, physical exam, imaging, and lab tests, helps identify the underlying cause and guide effective treatment.

Leave a Reply